Palliative Care in Thailand has been developed for over 20 years. The purposes of this study were to put together milestones of Palliative Care development in Thailand and examine events which were the turning points in level of development. After interviewing key experts in palliative care in Thailand, this study reviews published data on development approaches to palliative care and categorizes into 5 domains: policy, education in medical providers, public awareness, implementation, and drug availability. Development of Palliative Care in Thailand can be divided into 3 era: (1) dawn of Palliative Care (before 2004), (2) triangle that moves the mountain and health (2004-2012), and (3) the great leap forward (2012–present). Two significant events that are the turning points include activities where people across the country were connected to build the knowledge altogether, in 2004, and health promotion at the End of Life Projects and national palliative care association, both of which established in 2012, and an international palliative care conference hosted by Thailand in the same year. Thailand is transitioning to aged society, posing a challenge to the accessibility to palliative care in terms of both quality and quantity.
introduction
Palliative care in Thailand has developed continuously for nearly 20 years, considering the World Health Organization’s Public Health Strategy for Palliative Care framed in The development of palliative care in four areas, which are: (1) Policy, (2) Education, (3) Implementation, and (4) Drug availability(1), it was found that Palliative care in Thailand in each area has different development in different contexts over time and level of pushes from different sectors.
A comparative study of Palliative Care development at the International level by International Observatory On End of Life Care (IOELC) was pulled together from Palliative Care development information of each country around the world. A proposal of developmental stages of Palliative Care for each country has been developed into 4 groups, namely group of countries that not yet have Palliative Care, group of countries that at the preparation stage, a group of countries that have Palliative Care at regional level, and a group of countries that have Palliative Care in the mainstream health service (2).
Next, Worldwide Palliative Care Alliance (WPCA) has developed the country’s group division criteria and categorized countries in accordance with the development of Palliative care, by dividing country group number 3 and 4 into two additional sub-groups, so a total of 6 groups (3) as shown in Table 1.
Table 1 : Country Development Stage and Characteristics of Palliative Care as per Worldwide Palliative Care Alliance (WPCA)
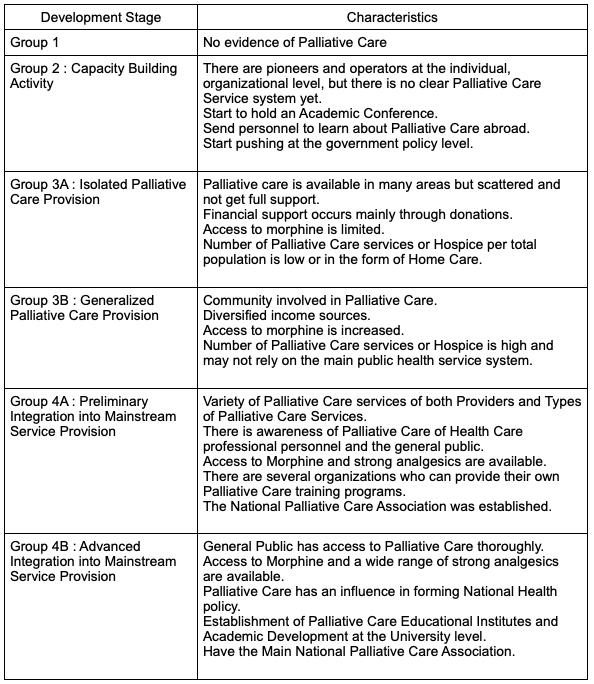
Thailand has been categorized as group 3a in 2013 and progressed to group 4a in 2017 according to the Palliative Care development criterias. (4) In addition, Thailand is ranked number 44th in the world in the Quality of Death by Economist Intelligence Unit (5) in 2015.
However, Thailand has made continuous progress in Palliative Care Development. It is worth noting that most of the Palliative Care information was recorded and organized in a variety of data sources and was recorded in Thai. There is a possibility that the information may not be included in the classification of Palliative Care Development of past studies. This article has the objective to combine important events that are related to Palliative Care in Thailand and study to outline and analyze the important turning points in development of Palliative care in Thailand.
The author has gathered the information related to the development of Palliative Care in Thailand from interviewing Khun Wanna Jarusomboon, President of the Peaceful Death Group. She has been on the path of Palliative Care development in Thailand and plays an important role in creating awareness in Thai society continuously from the beginning era to the present. And also interview Associate Professor Sri Wiang Phairotkul, President of Palliative Care and head of the Palliative Care Center, Srinakarin Hospital, Medical Faculty, Khon Kaen University who plays an important role in knowledge development, personnel building, and concrete Palliative Care services in Thailand. The author has compiled the developments of critical milestones, derived from interviewing both persons and searching for more related documents.
Then categorized the information according to various aspects of the Public Health Strategy for Palliative Care, covering all 4 aspects as per the World Health Organization, by separating the development into training/education of health care services providers; and general people public awareness. All together making a total of 5 aspects and summarizing the critical milestones throughout the development of Palliative Care in Thailand, as shown in Table 2.
Table 2: Critical Events in Development of Palliative Care in Thailand
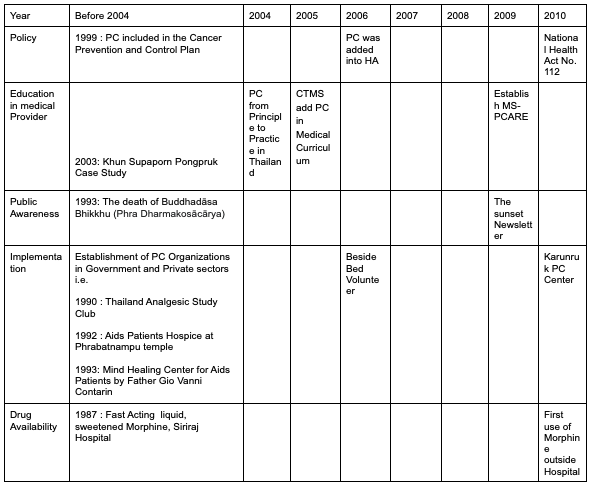
HA: medical Accreditation, MS-PCARE: Medical Schools Palliative Care Network
PC: Palliative Care
CTMS: Consortium of Thai Medical Schools
*2006: Palliative care is included in Hospital Standards and Medical Services for the first time.
** National Health Act No. 112 (Thai Living Will) BE 2550 (CA 2007)
Development of Palliative Care in Thailand
From collecting information on critical events and categorizing them into different categories as per the developmental aspects of Palliative Care, the author found that there is an event that seems to be a turning point that creates an accelerated level of development in two periods, making it possible to divide the development into 3 eras with details of the turning point event as follows:
The First Era : Dawn of Palliative Care (before 2004)
An important starting point that makes “death” a widespread debate in society was the death of
Phra Dharmakosācārya Buddhadāsa Bhikkhu (Nguam Indapañño) in 1993. That incident made the public start to give importance to Buddhist wisdom, considering death as natural, including raising important questions for the medical community of Living Will in refusing treatment that is only to prolong life. (6)
Khun Supaporn Phongpruek was another important case study, who created an important lesson in end-of-life care. She was the owner of “Ban Tua Phu”, a trainer, yoga teacher, translator and writer. She used Dharma to take care of her breast cancer by herself through meditation practice, cooked healthy food for herself and did not seek treatment in
hospital (7). In the end period when cancer spread more, Supaporn lived at her home among her friends who took turns to take care and organize activities in the house throughout the day. Meanwhile, the medical team led by Dr. Temsak Puengrasamee from the Faculty of Medicine
Prince of Songkhla University played a role in taking care of her symptoms at home until Supaporn passed away peacefully on October 18, 2003.
Ms. Supaporn’s case study showed that having a good death is something that can happen at home, with support and learning among family, friends and the community. At the same time, the medical team has learned about the possibility to design a health care system in managing suffering at the approaching death stage at home. And it is an example of a collaborative decision between the patient and physician on the treatment approach based on the value of the patient as the main concern (8). Therefore, Ms. Supaporn’s case study is regarded as a tangible upstream of Palliative Care, that is having good death can take place at home, by cooperation from family and social costs in the community. While the medical role must not be tied to the medical service provided in the hospital only. It is a joint decision between the “doctor” and the “patient” and supports the patient to die peacefully at home.
The Study of the “Death Paradigm Review Project and the Well-being Dimension” is the starting point for learning about death and the management of death in Thai society by Thana Nilchaikowit and team (9). It was found that the perspective on end-of-life care patients was not consistent across parties. The doctor sees it as a life-threatening condition, and cannot be completely cured. They just give drugs to control and manage symptoms and provide counseling to make patients and relatives accept the condition. At this period, the role of family and community is to visit and give support, be friends in suffering and happiness, ask for forgiveness, ask to share any unfinished matters, and take care of facilitating daily life and rituals. This causes communication gaps and limitations on access to information necessary to make decisions.
The organizations that initiated Palliative Care in this first period were widely distributed in both public hospitals and large private hospitals. The large hospitals include Songkhla Nakarin Hospital, Chulalongkorn Medical School Hospital, Siriraj Hospital, Ramathibodi Hospital, Pain Relief Clinic at National Cancer Institute. Community hospitals include Somdet Phra Sangkharat Hospital, Phra Nakhon Si Ayutthaya Community Hospital. Private sectors include Saint Louis Hospital, St.Clare’s Hospice Thammarak Niwet project that provides Hospice for end-of-life patients at Wat Phra Bat Nam Phu, Lopburi Province, etc. It was found that most private sectors had experiences in helping end-of-life patients, especially HIV-infected patients (HIV) and end-stage AIDS patients.
The Second Era : Triangle that Moves Mountains and Health (2004-2012)
In creating medical knowledge, health care professionals started to be interested in Palliative Care and work in their own areas according to their interests. In 2004, Faculty of Medicine Prince of Songkhla University organized Palliative Care Symposium: From Principles to Practice in Thailand at Songkhla Province. That creates opportunities for interested people from all over the country to exchange knowledge and experiences in all aspects and is regarded as the first specific academic conference at national level (10). After that, the group of medical personnel has got together making Palliative Care Network in Medical Schools (Medical
Schools-Palliative Care Network, MS-PCARE). In 2009, the health promotion medical school plan of the Consortium of Thai Medical Schools (CTMS) received funding from the Thai Health Promotion Foundation (ThaiHealth) with Dr. Temsak Puengrasamee, as the chairman of the network, created learning and exchanging experiences, teaching and workshops that rotated through network institutions. Such learning provided an opportunity to stimulate the host institution to publicize their Palliative Care work to interested internal personnel to form a network of collaboration within organizations and networks that come to work together such as volunteers, fellow patient – friend support friend group, Faculty of Nursing, etc. (11)
The three years of the Palliative Care network program in medical schools led to the creation of a draft Palliative Care curriculum that was integrated into the Doctor of Medicine (M.D.) curriculum, in which each of the 18 network institutions applied the draft to their own institutions curriculum (12) and produced textbooks to create integrated Palliative Care knowledge for end-of-life patients for interested general people (13-16). Moreover, there was research to study the need of Thailand Palliative Care and situations at that moment (17-19).
Around the same period, Buddhika Network led by Phra Paisal Visalo together with Samsikkhalai jointly developed the “Facing death peacefully” workshop, started in 2003 with funding from the Thai Health Promotion Foundation (ThaiHealth). The participants were from the general public and medical professionals, resulting in the knowledge accumulation of Palliative Care in all dimensions, case studies from Thai society, coupled with the production of learning materials, public forums, along with development of end-of-life care doctors and nurses network (20).
Therefore, it can be said that the period 2003-2004 was the period of a critical turning point where both medical professionals and people in Thai society began to form a Palliative Care learning group together, which was a shift from earlier periods in which each Individual or organization learned and worked independently. This resulted in an integrated learning network across the country.
“Facing death peacefully” workshops keep carrying on. There were interested people who attended the workshop and wanted to continue the work in Palliative Care but still lacked space to practice. Hence, Buddhika network initiated the “Beside Bed Volunteer” project in 2006 with support from the Thai Health Promotion Foundation (ThaiHealth) to increase the operational area for volunteers to play a role in taking care of patient’s mental, coordinate with a team of doctors and nurses on the in-depth information and create mutual understanding between patients and family (21).
In 2009, the Bhddhika Network organized “Sunset Newsletter” as a medium to gather knowledge and exchange work experiences about Palliative care, publicize activities and
communicate Palliative Care to general people, published continuously every 3 months and closed down in the year 2016 (22).
After the “Facing death peacefully” workshop continued for 5 years, a survey among people who have attended the workshop was conducted by Bhuddhika network. It was found that more than half of respondents were medical professionals who still lacked opportunity to practice knowledge or experiences in their Palliative Care work in the hospitals due to: (1) There is no time to do because Palliative care is not yet counted as main activities in the medical system in hospitals. (2) Colleges do not understand the palliative care process that consists of both science and art. (3) Leaders in the organization do not support, and (4) Lack confidence in applying knowledge and experience in real case.
To solve such problems, Khun Wanna Jarusomboon, manager of “Facing death peacefully” project, Bhuddhika network at that time anticipated that it was necessary to find a helper for the hospital system. Because the workload of medical professionals is very heavy, they are unable to provide comprehensive care for end-of-life patients in all dimensions, especially in the spiritual dimension. Meanwhile, Thai society has people in the community that have potential to help take care of those patients i.e. monks, monastics, nuns, volunteers, etc. These people can be critical helpers for medical professionals in the hospitals nicely. What is lacking is a system to bridge collaboration between communities and hospitals.
In 2011, the Bhuddhika network organized the “Promoting monks, hospitals and communities’ role in healing the mind of chronic and end-of-life patients project” in order to develop a Palliative care system that opens up space for the community or other sectors in society to participate or have an increased care-taking role. The key person who initiated the project is Phra Khanchit Akinchano, the abbot of Wat Virawongsaram, Muang District, Chaiyaphum Province (23). And it has continued in the second phase in the year 2014, under the project name of “Driving well-being wisdom dimension through caring for end-of-life patients” (24)
Overall, Health Care Professionals started to learn about Palliative Care from taking the course abroad, inviting oversea speakers to organize training in academic conferences and taking joint care of Palliative patients, until a group is formed into a Palliative Care network to learn about Palliative Care in the context of Thailand itself. At the same time, there is an initiative to drive and generate awareness of death to the general public. National policy related to palliative care didn’t play much role in the early stage. Government organizations that are involved in driving Palliative Care are medical Accreditation Institute (Public Organization) (HAI), whose role is to assess the quality standards of medical Service Institutions of all hospitals in Thailand. HAI added Palliative Care as part of the “standard”, causing the movement and the awakening of Palliative Care all over the countries. There is a mention of Palliative Care in the HA 60th Anniversary Celebration of King Bhumibol Adulyadej’s Accession to the throne Edition (25) in the year 2006, when at that time, there were still not many medical professionals who work on Palliative Care.
The National Health Security Office (NHSO) have launched projects to develop end-of-life care, promoting friendship therapy activity, friends help friends, and volunteer to support society in the year 2006 and has set that every District Office has to support hospitals in respective area, implement the pilot Palliative Care project for end-of-life patients in 2010(26).
Announcement of the National Health Act B.E. 2550 (B.C. 2007), as a master act published in the Government Gazette, has content that clearly supports Palliative Care, such as section 12 which is about giving opportunity to patients to refuse treatment that is solely for life-sustaining (27). At that time, there were obstacles in its implementation due to the awareness about end-of-life care was not yet widespread among both the medical and general public sector; and limited access to the Palliative Care services system, which is necessary to support patients in cases they do not receive treatment that is conducive to prolong life, but need support for sustaining life.
So it can be said that driving Palliative Care in this era is based on theory “Triangle moves
mountain” proposed by Prof. Prawet Wasi, M.D., who said that the strategy driving impossible things at the national level consisted of building knowledge, social movement, and connecting
to state power or political action (26). The Palliative Care network project in medical schools was the driver of the knowledge mountain. Bhuddhika Network, led by Phra Phaisan Visalo was the driver of the people sector through “Facing death peacefully” workshops. While the mountains of political movement and national policy have not yet played an important role but were a critical foundation in driving in the next era such as National Health Act of B.E. 2550 (BC 2007) section 12 which mentioned the letter of intent not to accept treatment that is to prolong life.
TheThird Era: The Great Leap Forward (2012–Present)
Thailand was proposed to host the Asia Pacific Hospice Conference (APHC) in 2013. It was the key event that stimulated the rapid development in Palliative Care and was considered to be an important international conference. Many countries in the Asia-Pacific region have taken the opportunity to organize such conferences to push for a Palliative care system in that country in a great leap forward such as Japan, South Korea, and the Philippines (28).
The Medical Schools Palliative Care Network (MSPCARE) was registered as Thai Palliative Care Society (THAPS) in 2012 to support the next year’s APHC. Thailand has the opportunity to host such an international conference. This has generated an alert and push of Palliative Care later on. Thailand Palliative Care Society (THAPS) implemented a well-being promotion toward the end-of-life project (29), with the fund supported by Thai Health Promotion Foundation (Thai Health). This is part of many projects, consisting of (1) The way to die peacefully awareness creation project (Death can talk), (2) create and manage knowledge of the health service system that enhance health project, (3) public health system study and development project in the end-of-life patients care with community participation and epidemiological studies, (4.1) Continuation project for Medical Schools Palliative Care Network, (4.2) Health Care Professional and Pharmacists Development Project, (4.3) Palliative Care Nurse Development Project, and (4.4) Volunteers and Caregivers Development Project.
Facing Death Peacefully Workshop and Volunteer Development Projects in the past era resulted in awareness of Palliative Care and death among certain numbers of the population but it was quite limited. This was driven by limited promotion and was accessible only to those with interests or has worked related to end-of-life patients. The way to die peacefully awareness creation project (Death can talk) run by the Buddhika network tried to communicate that death was something talkable in the society. They change the death image to be something tangible, not scary and not related to religion only. They also modified the way to do work, by working collaboratively with Advertising Agency and Creative to create varieties of creative work, such as music video clip, social media communication, and developed tools to help people talk about death, such as Life Unlock Card Games, Comfort Heart Book, etc. (30)
In October 2013, Bhuddhika Network and THAPS, with the support of Health partners, organized “Before I Die, Ready before die (31)” activity at the Central World Department store, which is an activity parallel to the APHC. There was lots of interest in the activity and there were hundreds of people participating at the department stores. This shows how death began to be of interest among the new generation and those who have never been involved in the death or end-of-life patients alone.
Subsequently, the “Death can speak ” project by Bhuddhika network, in collaboration with 18 network partners who work on learning about life and death, organized the “Happy Deathday” event at the Queen Sirikit National Convention Center, during June 10-11, 2017 (32). There were lots of people in new generations taking part and interested in activities. The participation of 18 organizations, which comprised of working people from both government and private sectors, have shown that caring related to end-of-life patients can continue according to its context. Wanna Charusomboon, President of Peaceful Death and Chairman of the Happy Deathday event commented that organizing such an event is a critical milestone that makes Thai society significantly aware of death preparation (33).
Great success of the “Happy Deathday” event led the “Death can speak” project to receive support from the Buddhika network to operate as an independent group with the name of “Peaceful Death” in 2018. Peaceful Death received funding support to implement the Compassionate Community for living and dying well from Thai Health Promotion Foundation (Thai Health) to develop the community’s potential to have an environment that is conducive to good death. The concept is that the loss experiences are the responsibility of everyone in society, relies on knowledge and skills of everyone in the community together with the support of the health system to be able to take care of end-of-life patients, enabling “Compassionate Community” to play a role of Palliative Care in social’s sector. In the present context, the number of patients requiring palliative care support is increasing, while the knowledge and understanding of taking care for this group of patients is still not thorough and health care professionals are not sufficient to meet the needs of the people (34).
In medical professionals, “Building and managing knowledge of public health service systems that promote well-being in the end-of-life stage according to Thailand’s context project” was mainly responsible by Dr. Temsak Puengrasamee, Faculty of Medicine, Songkhla Nakarin University. The project consists of 3 sub-projects (35) include Learning exchange forums, Community establishment, Community of Practice (CoP) on social network i.e. Facebook and GotoKnow, and gathering and synthesizing research data, thesis, media and related publications and preparing a database and compiled into “Thesis before death”. It is an accumulation of thesis or dissertation related to end-of-life patient care in Thailand from 1980 until 2016, with a total of 169 cases arranged according to topics and footnotes, summarizing the main idea of the relevant thesis (36).
Institutions that play a prominent role in providing comprehensive Palliative Care services and play a huge role in providing training to medical professionals in the following period is the Karunruk Palliative Care Center, Srinakarin Hospital, Faculty of Medicine, Khon Kaen University. It was established in February 2010 by Assoc. Prof. Sriwiang Pairojkul, M.D. as the head of the center and also the president of the Thai Palliative Care Society (THAPS).
Operations of the Karunruk Palliative Care Center in the early stages consisted of creating a comprehensive service system (service). It is a prototype institute, who for the first time, brought opioid medicine to use outside the hospital, enabling the opening of comprehensive Palliative care services.
In 2013-2014, the Karunruk Palliative Care center received funding support from the National Health Security Office (NHSO), the 7th Health Region and Thai Health Promotion Foundation (Thai Health) to provide training for doctors and nurses. This resulted in a strong network starting from the 7th health region, then expanded to cover the Northeast region. The 4 weeks Clinical Palliative Care for Community Nurses Training (CPCN) made the referral of end-of-life patients in the Northeast region to have ability to cover all areas. They can pass on the medical information and have the same practice guidelines, creating a seamless patient care system, which is the heart of Palliative Care and can take care of patients to die at home according to needs of patients and families.
Until 2018, the 4-week Clinical Palliative Care for Community Nurses Training expanded the Palliative Care network to cover hospitals in the North and South regions. Also, the curriculum of ‘how to set PC programs in your hospital’ is the foundation of the Palliative care establishment in hospitals.The expansion of the PC network from the Northeastern region to the nationwide is driven by Karunruk Palliative Care Center.
Operations that go along with comprehensive services and a strong network make Karunkuk a complete Palliative Care Center, which is suitable to use as a model area for training for medical professionals. Karunruk started a long term 6 weeks nurses training curriculum, named ‘Basic Certificate Course in Palliative Nursing’ (BCCPN) in 2011 and continues until now. Assoc. Prof. Sriwiang Pairojkul, M.D. found that nurses who had undergone this long-term training had an important role in driving the establishment of Palliative Care Centers in many large hospitals across the country, including many Medical School hospitals. However, due to the limited roles and responsibilities of nurses, driving Palliative Care Centers requires physicians in prescribing medication for symptoms treatment, including connection to specialized care in other fields. This must leverage physicians roles in proactive work. Therefore, Karunrak Palliative Care Center has developed a long-term 8-week course for doctors, named ‘Basic Certificate Course in Palliative Medicine’ (BCCPM) in 2014. Trained doctors and nurses have become a leader to drive change and manage Palliative Care services in various hospitals across the country.
Since 2014, there is increasing training for medical professionals to support the increase in numbers of medical professionals required to support Palliative Care. Thai Palliative Care Society (THAPS) have provided funding for organizing additional training courses in a wider range of topics (37). This made Palliative Care become well known in the medical community in more and more specialist areas.
The Training Curriculum specialized in Palliative Care was created in 2019 as a certificate program of Medical Proficiency in Palliative Care in Family Medicine, under the responsibilities of the Royal College of Family Physicians of Thailand. The curriculum duration is 1 year (38). Now the curriculums are available in 5 institutions, including the Faculty of Medicine Siriraj Hospital, Faculty of Medicine Ramathibodi Hospital, Mahidol University, Faculty of Medicine Chulalongkorn University, Faculty of Medicine Khon Kaen University and the Faculty of Medicine Chiang Mai University.
The Palliative Care drive at national policy level after APHC conferences in 2003 is a national strategic plan for health promotion at the end-of-life stage, 2014-2016, which has got approval by the National Health Board. The purpose is to serve as a systemic tool leading to end-of-life health promotion (39). And in 2016, the Ministry of Public Health established a policy for every hospital to provide Palliative Care to patients and set it as a Service Plan Palliative Care in 2017 (40), which aligned well with accelerating the development of medical professionals and nurses in providing Palliative Care through continuous training by the Thai Palliative Care Society (THAPS).
Though Palliative Care is under the Ministry of Public Health service plan system, which resulted in the establishment of a Palliative Care Centers in every hospital, the quality of services need to be evaluated and developed. Assoc. Prof. Dr. Sri Wiang Pairojkun and the Palliative Care Network of Thailand jointly established the Quality Standard for Palliative Care with a self-assessment handbook in 2018 for use in assessing and developing quality of Palliative care centers. The Department of Medical Services has distributed them to Palliative Care centers across the country to use as a standard in operation and to assess development gaps and lead to quality improvement (41).
Base on the Health Data Center from the Ministry of Public Health in fiscal year 2021 compared to fiscal year 2019, it was found that patients receiving Palliative Care Support aged under 15 years old is at 14.88% from 9.40% respectively, teenager to working age patients is at 34.03% from 33.65% respectively, and the elderly of 60 years and over is at 28.38% from 25.56% respectively (42). And from a point prevalence study across 14 hospitals nationwide by the Palliative Care network of Thailand, the prevalence of terminally ill patients was 18.72%, separated into cancer group 55.66% and other non-cancer chronic diseases 44.44%(41).
Only 6-17% of end-of-life patients receive counseling and care by Palliative Care Centers in Tertiary care hospitals (41, 42). Of the group who received care from the Palliative Care Center, It was found that there were 88.7% who have an Advance Care Plan, compared to 15.7% of the group of patients who were not taking care by the Palliative Care team. The Health Data Center from the Ministry of Health in 2021 revealed that at an overall national level only 50.5% of end-of-life Palliative Care patients had family meeting activity and did an Advance Care Planning together with patients and families (43).
In the medical personnel survey in 2012 (18), it was found that there were 12 doctors who passed the more than 1 year Palliative Care training and 6 passed the more than 1 month training. Total number of doctors who passed Palliative care training nationwide is 147 people after the establishment of the Karunrak Palliative Care center and training for medical professionals. Throughout the year 2010-2019, there are 189 doctors who have passed the medium-long term training course, divided into 29 doctors who passed the 1 year mid-career training course and 160 doctors who passed the 8-week BCCPM courses (44).
In the medical personnel survey in 2012, it was found that of the total 1,680 nurses, only 49 nurses have completed the long-term training course of more than 1 month, accounting for 3%. Later in the year 2010-2019, Karunrak Palliative Care Center organized a training course for another 927 nurses, divided into 6 nurses who passed 1 year mid-career training course and 174 nurses passed the 6-week BCCPN course (44).
Study by Thailand Development Research Institute, TDRI in 2020 (45) about public awareness and attitudes among 2,394 Thai people aged 20-80 years toward Palliative Care, found that only 43% were aware of end-of-life care. Most of them are elderly people or those who have chronic diseases. Only 24% were aware of Palliative Care and found that more than 92% were aware of the National Health Act B.E. 2007 Article 12 about the right to refuse treatment that intend to prolong lives. But only 14% of them have prepared their own Life Will or Advance Health Care Plan. This shows that there is a gap in raising awareness about Advance Care Plan for the overall general public.
Method of Study
The development of Palliative Care in Thailand in the past 20 years can be divided into 3 eras:
the First Era: Dawn of Palliative Care (before 2004), the Second Era: Triangle that Moves Mountains and Health (2004-2012) and the Third Era: The Great Leap forward (2012–present). An important turning point is organizing an academic conference on Palliative Care and the “Facing Death Peacefully” project, pulling together medical personnel and people as a network to create knowledge and common vs. separated working areas. The second turning point that made Palliative Care development to the great leap forward in the third era is health promotion at the End of Life Projects, the establishment of Medical School Palliative Care Network and organizing the APHC conference which Thailand is the host. All these three events are the critical causes that accelerated learning and Palliative Care in all dimensions
From the compilation of Palliative Care History in Thailand, the author found that interviewing two experts who play a key role in driving Palliative Care makes the author see the whole picture and continuation of important events that affect each other. And these correlational data were not previously recorded. In the process of searching for relevant documents from the stories collected from the interview, the author found that the data source was dispersed and some data was recorded by operators in the form of private notes in Thai on the Internet. Data about driving general people perception has been collected completely on the website of the Buddhika network, showing a continuous drive from “Facing death peacefully” until “Compassion Community for Live and Die Well” by Peaceful Death. Author has limited search capacity when it comes to data sources related to policy and government documents, this may result in incomplete Palliative Care development in terms of policy.
At present, Thai society is transitioning into an aging society and the social structure is more urban, creating challenges for the direction of Palliative Care in the future. Characteristics of a “Good Death” in new generation context may not be the same as the original set of beliefs we are familiar with, based on the statistical data of the Palliative Care situation at present vs. the past. As mentioned above, a gap of Palliative Care Development in Thailand would consist of (1) Increasing access to Palliative Care Services, (2) Increasing awareness of doctors in different fields on the role of Palliative Care, (3) Establishing a structured system for Palliative Care to be equivalent to other specialized care, (4) Assigning full time roles for Palliative Care personals, with a clear career path, (5) Increasing involvement of the private sector, civil society and the general public sector in terms of Palliative care, (6) Efficacy and effectiveness studies of current Palliative Care, (7) Research study on alternative medicine that has potential in taking care of palliative care patients that the general public can access, such as medical marijuana. All of these will be factors that help reduce the barriers to access such services for all patients thoroughly and with quality. When life and death are part of life and shared responsibility of citizens, the future of Thailand’s Palliative Care is therefore determined by all Thai people.
Acknowledgment
The author would like to thank Khun Wanna Jarusomboon and Assoc. Prof. Dr. Sriwiang Pairojkul deeply for the interview and powerful described the path of Palliative Care experiences. Gathering events on various data sources, making the author realize that there are many more people who participated in the creation of Palliative Care in Thailand that the author can not mention them all here. Caring for a fellow human being to pass away peacefully is so valuable and creates a good meaning for that person himself, and with those around him who are still alive. The author, therefore, would like to pay homage to everyone who is involved in creating value for Palliative care, both named and unnamed.